The latest data from the UK Health Security Agency shows that diagnoses of gonorrhoea and syphilis have surged in the last year. Shockingly, gonorrhoea rates are the highest they have been since records began in 1918.
Gonorrhoea has increased from 71,133 diagnoses per year before the pandemic to 82,592 in 2022. It’s now the second most commonly diagnosed STI behind chlamydia. In people aged 15-24, rates of gonorrhoea almost doubled in 2021 compared to the year before. Syphilis, which in the early 2000s was almost non-existent in the UK, has increased to 8,692 diagnoses in 2022.
Both these sexually transmitted infections were known by Victorian society. Syphilis was especially feared because of the visible and debilitating symptoms it causes. But the advent of testing and antibiotic treatment has meant most people have forgotten about them – and the risks they can pose.
What symptoms do they cause?
Gonorrhoea
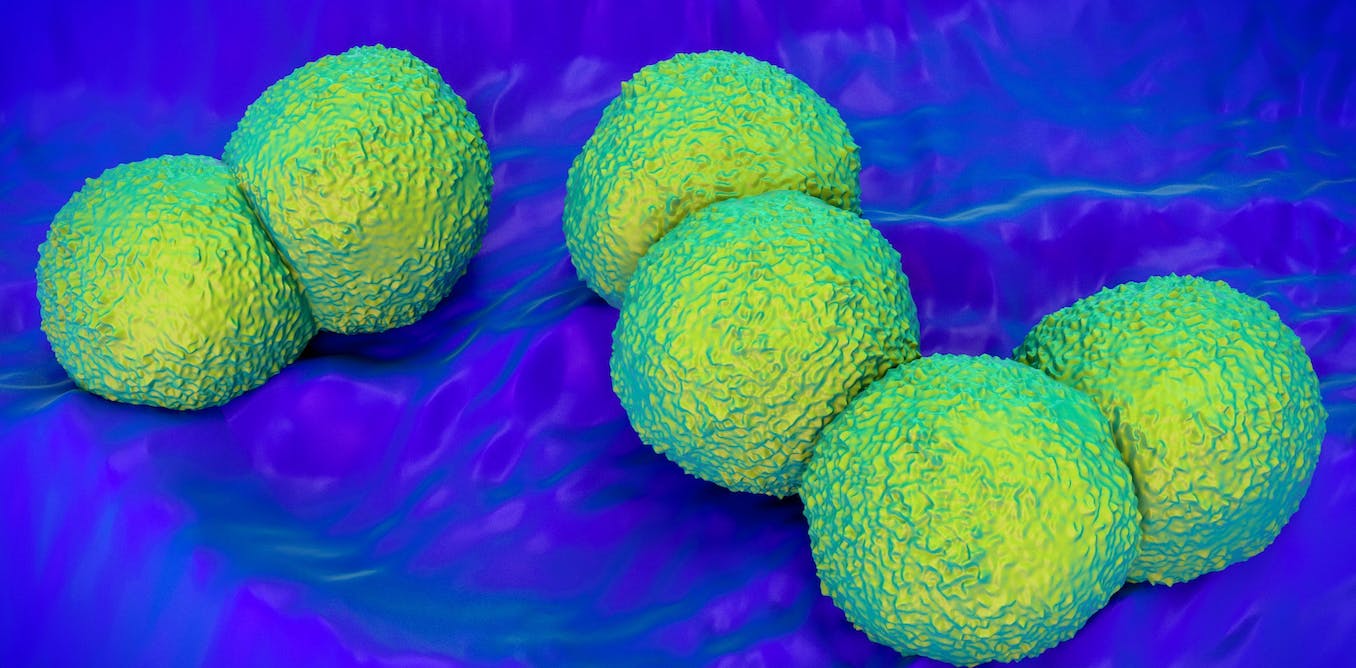
Gonorrhoea is caused by a small round bacteria called gonococcus which infects the urethra, testes, prostate and anus in men, and the vagina, cervix, womb and anus in women. It’s passed from one person to another during unprotected sex.
Untreated, it causes a pus-filled discharge or “drip” from the penis and severe pain while urinating. In women symptoms can be less obvious, but include a watery, green, yellow or sometimes bloodstained vaginal discharge, and pain when urinating.
If the infection spreads to the womb and ovaries this causes pelvic inflammatory disease. Symptoms include fever and abdominal pain. Pelvic inflammatory disease is treatable but can lead to long-term complications even after the infection has subsided – including fertility problems and greater chance of ectopic pregnancies.
Gonorrhoea used to be easily treated by antibiotics. But in the last ten years, several extremely drug resistant strains have been detected worldwide (including in the UK), making some infections difficult to treat. Drug resistant strains can happen when an infection is partially treated with the wrong antibiotic, or if a person stops treatment before the infection is completely gone. There’s a real and frightening risk that gonorrhoea could become untreatable once again, as it was in the 19th century.
For this reason, it’s essential to get diagnosed and treated if you’re experiencing any symptoms. Current treatment involves an injection of a single antibiotic alongside close follow-up to ensure the infection is eliminated.
Syphilis
Syphilis is much less common than gonorrhoea, but it can cause much more harm.
The infection is caused by a small spiral bacterium called Treponema pallidum. Without treatment, this bacterium stays in the body and can cause complications that can happen 20 years or more after the infection.
It can also be passed from mother to baby in the womb, and can cause stillbirth or congenital syphilis. This means the child is born infected with syphilis and may develop the unpleasant complications of the infection in childhood. Every pregnant woman in the UK is screened for syphilis. If detected, the mother will be treated – which also protects the baby from harm.
Syphilis causes three stages of disease. The first stage is a painless lump or ulcer on the genitals or infected area. This usually goes away in a matter of weeks. The second stage is a full-body rash, sometimes with a sore throat and swollen lymph glands. These symptoms can also settle without treatment, though the person remains infected and infectious. The disease now enters a latent phase where it stays in the body while showing no symptoms. It can also still be passed to sexual partners or from pregnant women to their babies.
Peddalanka Ramesh Babu/ Shutterstock
In about a third of infected people who are untreated, the disease can return after a number of years as the third stage of tertiary syphilis. This causes a range of symptoms which were dreaded in the years before effective treatment – including skin and bone disfigurations, nerve pain, heart problems, deafness, blindness, dementia and other neurological symptoms such as difficulty walking and incontinence.
Fortunately syphilis is still very treatable using penicillin or similar antibiotics. As you might expect, once a case is diagnosed, great efforts are made not only to cure the affected person, but to trace and screen sexual partners – going back many years if necessary.
Why have rates increased?
It’s not entirely clear why rates of syphilis and gonorrhoea have increased so rapidly in the UK. In part it may be due to a “bounce back” from the restrictions of the pandemic years, and the fact that people were not able to access diagnosis and treatment as readily during that time.
Young people may also have missed out on sex education during the pandemic and may not know how to properly protect themselves from STIs.
Sexual health services in England have also experienced funding cuts – making it more difficult for some people to access sexual health advice, diagnosis and treatment. Data shows that rates of gonorrhoea in particular are sensitive to social and political change, including changes to funding for sexual health services.
What can I do to protect myself?
The best way to protect yourself and your partners against gonorrhoea or syphilis is to get tested before starting a new relationship, and to use condoms with new or casual sexual partners.
If you have a symptom you’re worried about, get it checked. Self-test kits for gonorrhoea and syphilis are available online in some areas or you can go to a sexual health clinic if you prefer.
If you’re notified by a partner or clinic that you’ve been in contact with someone who’s been diagnosed with one of these infections, attend a clinic to get screened and treated if necessary.
We’re fortunate that both syphilis and gonorrhoea are still treatable once diagnosed. But it’s important to know about them and to get tested and treated promptly.