|
Getting your Trinity Audio player ready...
|
As countries in the northern hemisphere face a bitterly cold snap, there is serious risk of injury – and even death – from freezing weather.
Thankfully, with the right preventative and protective measures, the human body can survive these icy temperatures.
Here’s what you need to know about identifying and treating the most common cold injury: frostbite.
The body runs most optimally at 37°C and has a number of inbuilt mechanisms to adjust to cold or hot changes in environments.
These include changing our breathing rate, adjusting blood supply to various areas of the body or altering our fluid intake to ensure we replenish what we lose through respiration, exertion and urination.
However, despite our bodies’ inherent temperature controls, without the right protection, we might still be vulnerable to cold weather injuries.
Frostbite is the result of damage to tissues – usually skin – on exposure to subzero temperatures.
Most commonly damaged areas are ears, fingers, toes, cheeks, lips, nose and other extremities that are exposed – or not covered enough – such as the penis in winter sports or the eyes.
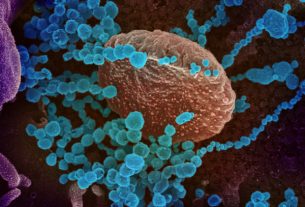
GOPEN RAI/AFP via Getty Images
For frostbite to occur, exposed body parts need to be subjected to a temperature that is below minus 0.55°C. At this temperature it will take several hours for exposed skin to become frostbitten.
But length of exposure to the cold is not the sole factor. The further below zero the temperature, the quicker the onset of frostbite.
Windchill has a significant impact on the likelihood of getting frostbite too. For example, temperatures in the -20s can cause frostbite on exposed skin in under 30 minutes.
Wet clothing also increases the risk of developing frostbite: the moisture removes heat away from the body far quicker than air does, reducing the time taken to develop it.
Who does it affect?
Frostbite is seen more commonly in men and is increasingly found in certain occupational groups such as farming and fishing professionals, mountaineers, manual labourers and the military. However, with the global population beginning to live in harsher environments and an increase in winter and snow sports, this is likely to increase in the general population.
Those who are diabetic or pre-diabetic are also at increased risk, not because of their inability to metabolise glucose, but because damage to the nervous system means they are less likely to feel and respond to the cold. Reduced ability to sense the cold also increases the frostbite vulnerability of those who’ve had a stroke or have peripheral nerve damage.
People with heart conditions are also more at risk because the cold, especially the wind, takes the heat away from the body placing increased strain on the heart, which must work harder to keep warm.
Significant alcohol consumption is a further risk factor for frostbite. Heavy intoxication inhibits the body’s protective response to low temperatures and can result in the sufferer not recognising the pain and discomfort as an early warning sign of cold damage.
The consumption of alcohol also reduces blood pressure, which may also reduce the amount of blood pumped to extremities.
Symptoms
Cold weather causes exposed skin temperature to drop, which triggers a response from the body to reduce the blood flow – known as vasoconstriction – to these cold areas to maintain core body temperature. Preserving the core body temperature is key to keeping the brain, heart, kidneys and lungs functioning and preventing hypothermia.
Withdrawing blood from the extremities reduces the risk of ice crystals forming in blood, however, over time with continued exposure to the cold, the water in the tissues begins to freeze, causing ice crystals to damage the tissues.
This cooling brings about tingling and numbness of the exposed areas, and skin flushes red or white as the body frantically tries to rewarm itself.
This initial stage is known as frostnip, and, although uncomfortable, leaves no permanent damage to tissues. Beyond this stage, tissues begin to freeze.
If only the skin and the underlying connective tissues are frozen, this is termed superficial frostbite. The skin turns pale or even greyish blue because of decreased blood flow, ice crystal formation, limited blood supply – and there’s total numbness in the affected areas.
As exposure progresses, the freezing of tissue moves deeper involving muscles and tendons, blood vessels and even bones. This level of freezing is deep frostbite and is associated with more extreme outcomes, such as amputation.
Treatment and prevention
For frostbite, immediate medical treatment should be sought – sadly the pain of recovery is often far worse than the injury.
Rewarming is the process of bringing the affected parts back to functioning body temperature. However, where ice crystals have damaged tissue, blisters are common and the nerves become hypersensitive, causing excruciating pain.
In severe cases, debridement surgery may be needed to remove dead tissue.
In the most extreme cases, however, there is the possibility that the affected area cannot be saved and requires amputation – if the tissue hasn’t already died and fallen off.
During this cold snap, if you have to go out in the cold weather, minimise your time outside.
Ensure that you have multiple layers on, this minimises heat loss. Wearing anything to provide a barrier to your extremities to the cold. Hats, gloves and scarfs can protect the areas most affected by frostbite.