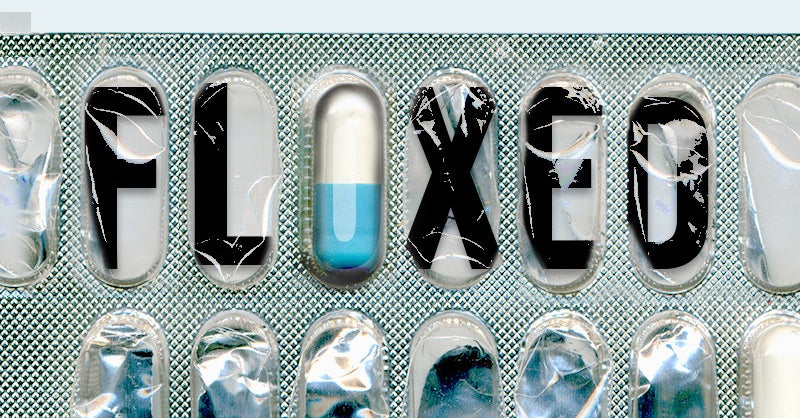
R&B singer Bobby Caldwell died this week reportedly after experiencing several years of health problems associated with taking a fluoroquinolone antibiotic, something referred to as being “floxed.”
The legendary musician, who sang “What You Won’t Do For Love,” died at age 71.
His was not an isolated case. The FDA has even dubbed the constellation of rare symptoms experienced by some people as fluoroquinolone-associated disability or FQAD and posted boxed warnings on the label. Some newer fluoroquinolones have been withdrawn from the market due to toxic effects.
Although all drugs have potential side effects, these seem to be different in their sheer variety and severity. Since fluoroquinolones were first introduced in the 1970s, problems have included cases of tendonitis, a swelling of tendons that can lead to ruptures; headaches and rashes; aortic aneurysms, which can be life-threatening; neuropathy, a type of nerve damage; high blood sugar; and anxiety.
Caldwell’s symptoms were reportedly nerve-related and started with a ruptured Achilles tendon after being prescribed medication in 2017.
What are fluoroquinolones?
Fluoroquinolones refer to a class of antibiotic medications that includes ciprofloxacin (Cipro), levofloxacin (Levaquin), and moxifloxacin (Avelox). They’re among the most widely prescribed antibiotic drugs in the US. They’re frequently used to treat sinusitis, bronchitis, urinary tract infections, and pneumonia along with gastrointestinal infections like gastritis and diverticulitis, according to William L. Musick, a pharmacist and clinical specialist in infectious diseases at Houston Methodist Hospital.
The drugs are life-saving in many cases and, unlike many other antibiotics, can be used easily both in and out of hospitals.
“Very sick patients inside a hospital can use intravenous formulations but also oral formulations outside,” Musick said. “That made it very easy to treat someone aggressively inside the hospital and give them a pill to take at home to finish the course. Unfortunately, we don’t have a lot of antibiotics that meet that criteria.”
They’re also effective. “They’re wonderful antibiotics. They can eradicate many infections, even anthrax, and they’re also very cheap to manufacture,” said Cecilia Bove, an assistant professor of biology at York College of Pennsylvania. Bove has researched and published on the subject.
What does it mean to be “floxed”?
Once the drugs reached the market and were used by millions and millions of people as opposed to the hundreds or so in clinical trials, some of the rare side effects inevitably appeared. It took a while, though, with the first label change (related to the risk of Achilles tendon rupture) not happening until 2004, so almost 30 years after the drugs were introduced, Bove said.
Most drugs go through a similar cycle (Vioxx and Celebrex, the pain reliever drugs, are prime examples), but the fluoroquinolones seem to be different in the variety of rare problems connected with them.
There are musculoskeletal problems like tendon ruptures but also psychiatric effects, aortic aneurysms, nerve problems, blood sugar issues, and digestive problems, which collectively resemble a syndrome more than individual side effects, Bove said.
The other difference is that many of the side effects last a long time. Some have even been permanent. “Researchers noticed a group of patients who would suffer for up to two or three months, if not more, of a constellation of side effects that lasted way after terminating the drugs,” Bove said.
“Unless it’s an event like a heart attack that can have lasting consequences, doctors are often unaware that side effects can not only outlast the period of the drug, but new problems can emerge and evolve after a drug has been stopped,” said Dr. Beatrice Golomb, professor of medicine at the University of California, San Diego, School of Medicine. “For instance, someone might start with a ruptured tendon then develop fatigue then neuropsychiatric symptoms following FQ use.”
Why are the symptoms happening?
There’s still a lot we don’t know about why fluoroquinolones have these effects in some people.
On a basic level, it seems clear that in addition to depleting bacteria, the antibiotics are also attacking the human body, Bove said. For instance, they may be destroying collagen and preventing repair, which would explain the effects on tendons, she added.
Her research team and others are still trying to find a common denominator that would explain the effects on different physiological systems.
“It’s been an underserved area in research because not many people have it,” Bove said. “It’s a rare disease, though it may be underreported due to lack of a diagnostic criteria.”
Fluoroquinolone-associated disability
In trying to characterize FQAD, the FDA has stated that effects have to disrupt a person’s ability to conduct the tasks of daily living and must last at least 30 days after stopping use of the drug. There also need to be symptoms in at least two of these body systems:
- Musculoskeletal
- Neuropsychiatric
- Peripheral nervous system
- Senses (vision, hearing, etc.)
- Skin
- Cardiovascular
Who’s at risk?
It’s not entirely clear who’s at risk for having these symptoms. The FDA’s adverse-event reporting system of cases between 1997 and 2015 indicates that about three-quarters of cases occur in people 30 to 59 years old, with most seen in women.
One study of almost 50 million antibiotic prescriptions in US adults identified a troubling rise of aortic aneurysms within 90 days of using a fluoroquinolone (as opposed to another antibiotic), but there didn’t seem to be any patterns in age, gender, and underlying health except that those affected were 35 years and older. (The study found an association but it couldn’t prove that fluoroquinolones were the direct cause.)
Aortic aneurysms occur when the inner lining of the largest blood vessel in the body separates from the outer lining, fills with blood, and balloons out in a way that increases the risk for a dramatic and life-threatening rupture.
Overuse of fluoroquinolones
Like many antibiotics, fluoroquinolones seem to be overprescribed.
A study conducted by the CDC and published in 2018 found that 5.1% of outpatient fluoroquinolone prescriptions for adults were for conditions that didn’t need antibiotics at all, while almost 20% were for conditions that should have been treated with another antibiotic.
“They are so easy and convenient to use in both the inpatient and outpatient setting,” Musick said. “I feel strongly that’s one of things that led to their abuse on the outpatient side. Other options have been pushed aside.”
“Most who go on to develop these serious problems had at least minor side effects during or immediately after FQ use. However, most with minor side effects do not go on to develop chronic problems,” added Golomb, who was the lead author of a report on four previously healthy adults who had experienced these adverse effects. “Often, it’s young, active people with no chronic health problems. And often it was people who never should have been on an antibiotic in the first place.”
What to do
Future efforts to reduce the incidence of these effects will probably have more to do with prevention than treatment. But fluoroquinolones may be more useful for very sick patients in hospitals rather than people who are able to stay home, Musick said.
“The labels clearly state that those drugs should not be given for simple infections that could be treated by other antibiotics,” Bove said. “Doctors still prescribe them for something as simple as a urinary tract infection.”
“There are multiple options for treating many infections and the first thing in the world of antimicrobial stewardship is “Does the patient really need antibiotics for what they have?” Musick said.