|
Getting your Trinity Audio player ready...
|
New York City prostate cancer surgeon, Dr. David Samadi, discusses findings from recent report of concerning increase in prostate cancer mortality rates
— Dr. David Samadi
NEW YORK CITY, NY, UNITED STATES, February 27, 2023 /EINPresswire.com/ — Let’s start with the good news first: There was a continuation of a 33% decline since 1991 in the overall number of U.S. cancer death rates, according to the American Cancer Society’s (ACS) annual statistics report. However, despite this encouraging news, this did not apply to prostate cancer deaths among American men. Instead, it increased by 3% yearly from 2014 through 2019 after two decades of declines. For me, a New York City urologist and prostate cancer surgeon, this disappointing news reinforces that additional work, educating men and their families about this second leading cause of cancer death among U.S. men, is imperative.
Prostate cancer estimated stats for 2023
The ACS estimates that 288,300 men will be diagnosed with prostate cancer this year. This number means almost 20,000 more men will be diagnosed with the disease than the number of men diagnosed in 2022. Higher rates of advanced prostate cancer are driving most of this downturn in prostate cancer rates.
A particularly concerning finding was that black men have been and will continue to be primarily affected by the increase in prostate cancer. This annual statistics report from ACS stated that black men have a 70% higher risk of prostate cancer than white men. In addition, black men have a two- to fourfold increase in deaths from the disease, a higher rate than any other ethnic group in the U.S.
Advanced prostate cancer diagnoses have also seen a 5% year-over-year increase which means one thing: Men are not getting prostate cancer screenings to catch this disease at an earlier, more treatable stage. ACS officials stated this is likely from confusion and continued debate over screening guidelines.
Screening tools for detecting prostate cancer
There are two tests commonly used to screen for prostate cancer:
1. Prostate-specific antigen test or PSA blood test.
2. Digital rectal exam or DRE test
Each test helps screen for possible prostate cancer conducted at a doctor’s office. The best time to find this disease is at its earliest, most treatable stage. Men diagnosed with early-stage prostate cancer have an outstanding 98-99% survival rate. Conversely, prostate cancer that has metastasized or spread beyond the prostate gland or is more advanced at the time of diagnosis makes treatment more complex, with lower survival rates.
The PSA blood test can detect the amount of protein the prostate makes. Men with a high level of PSA in their blood may indicate prostate cancer, but it is not foolproof. Other factors, such as an enlarged prostate or prostatitis, can also increase PSA levels.
During a DRE exam, a doctor checks the rectum feeling for any lumps or bumps on the prostate gland. Unusual findings on the PSA or DRE tests may require further testing for an accurate diagnosis of prostate cancer.
Special recommendations for men
As a urologist oncologist with over 20 years of experience treating and caring for men with prostate cancer, I recommend all men at age 40 have a baseline PSA test. In addition, any man with a family history of their father or brother diagnosed with prostate cancer or a female relative with breast cancer caused by the BRCA2 gene should begin at age 40. These men will be at a higher risk for not only developing prostate cancer but also for developing aggressive prostate cancer.
Men with an abnormal finding from a PSA or DRE exam would benefit from a diagnostic technique called magnetic resonance imaging (MRI) fusion biopsy. MRI fusion biopsy provides a more accurate diagnosis for the determination of prostate cancer. This tool has dramatically changed how we diagnose prostate cancer and whether to go ahead and biopsy.
My other concern is reversing the differences between black men versus white men and prostate cancer diagnoses and death rates. The ACS has a plan called Improving Mortality from Prostate Cancer Together (IMPACT) to reduce death rates among black men by 2035. This plan includes improving education, new research programs, and a second look at prostate cancer screening guidelines.
Final thoughts
With new diagnostic tools and efforts to reduce prostate cancer rates and mortality, the future of fighting this disease with prevention, detection, and early treatment for all American men looks more promising.
References:
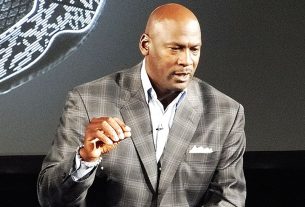
Dr. David Samadi is the Director of Men’s Health and Urologic Oncology at St. Francis Hospital in Long Island. He’s a renowned and highly successful board certified Urologic Oncologist Expert and Robotic Surgeon in New York City, regarded as one of the leading prostate surgeons in the U.S., with a vast expertise in prostate cancer treatment and Robotic-Assisted Laparoscopic Prostatectomy. Dr. Samadi is a medical contributor to NewsMax TV and is also the author of The Ultimate MANual, Dr. Samadi’s Guide to Men’s Health and Wellness, available online both on Amazon and Barnes & Noble. Visit Dr. Samadi’s websites at robotic oncology and prostate cancer 911.
David Samadi
Madison Urology
+1 212-365-5000
email us here
Visit us on social media:
Facebook
Twitter
LinkedIn
Instagram
YouTube
What is a PSA Test?
![]()