It wasn’t that long ago that some people speculated that long COVID was all in the mind – a psychosomatic illness. Thankfully, that period of speculation is now behind us. We have compelling evidence that long COVID is very real and very harmful.
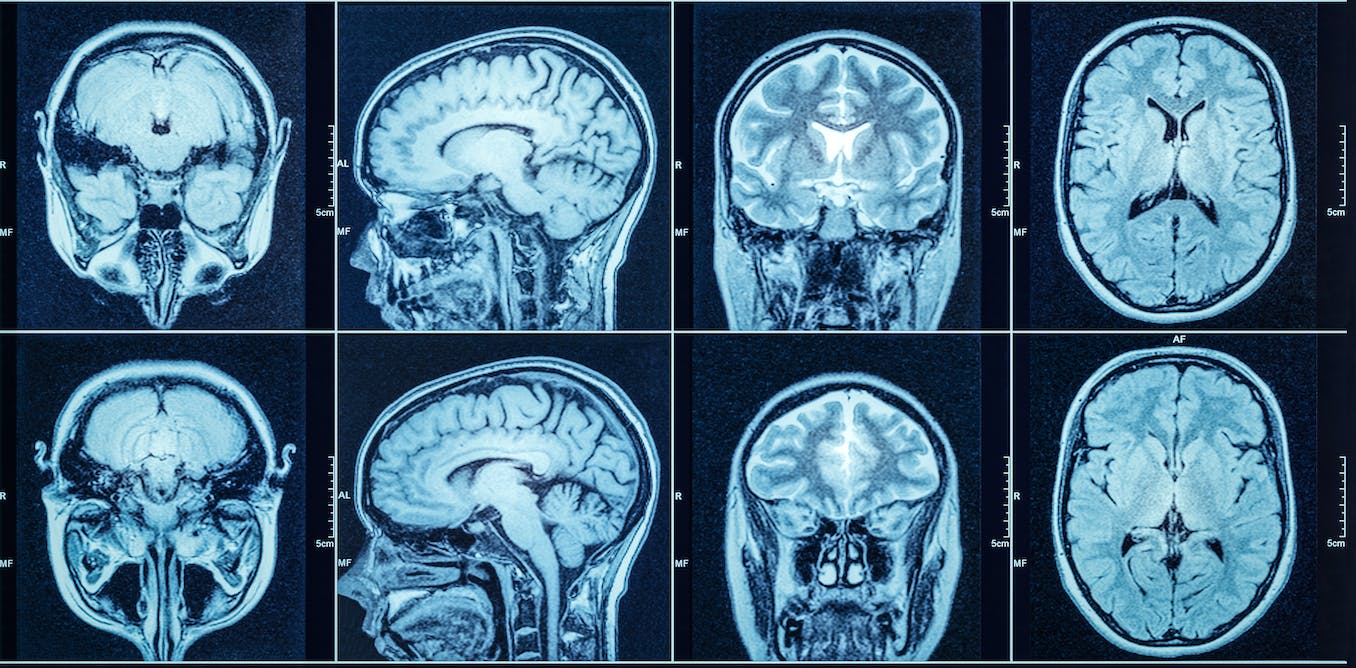
I’m the lead investigator on an ongoing study called C-More which looks at the long-term harms caused by COVID. Our latest findings, published in The Lancet Respiratory Medicine, show that nearly a third of people who were severely ill with COVID have multiple organ abnormalities on MRI five months after they were discharged from hospital. This is based on a sample of 259 people who were hospitalised with COVID and 52 in the control group who did not catch COVID.
MRI scans revealed that people with long COVID were 14 times more likely to have lung abnormalities than people who never had the disease, three times more likely to have brain abnormalities and two times more likely to have kidney abnormalities. The extent of MRI abnormalities was linked to the severity of their COVID, their age and whether or not they had other diseases.
People with long COVID who had abnormalities involving more than two organs were four times more likely to report “severe” or “very severe” mental and physical impairment.
In the beginning
When COVID first emerged, doctors perceived it to be a respiratory illness, with patients reporting pronounced coughing, shortness of breath and symptoms akin to pneumonia. But as our global understanding of the disease evolved, so did our appreciation of this complex disease.
Reports began to emerge that the virus was capable of not just affecting the lungs but also other organs, such as the heart, kidneys, brain and blood vessels, causing a broader assault.
Studies identifying the viral proteins in various organs also began to emerge, demonstrating the virus’s fondness for certain tissues that were not part of the lungs.
Originally, the main theory put forward was that SARS-CoV-2 (the virus that causes COVID) was directly infecting cells across multiple organs. But, as data accumulated, a more nuanced understanding emerged. It was observed that in some patients, the immune system, in its defence against the virus, overshot its response, leading to what’s termed a “cytokine storm”. This hyperactive immune reaction wasn’t always discriminative, causing unintended damage to organs not directly under viral attack.
KaliAntye/Shutterstock
Further reports highlighting the predisposition of the virus to induce excess clotting, mitochondrial disruption (mitochondria being the powerhouses of our cells) and reactivation of other viruses emerged. More importantly, there was a growing number of patients continuing to report persistent disabling symptoms arising from multiple organs, even after surviving the initial infection, also known as long COVID, a condition now thought to affect one in ten people.
So the narrative shifted. COVID wasn’t merely a short respiratory affliction, but a multisystemic disease with the potential for long-term complications, challenging our assumptions about how to treat the disease.
The birth of C-More
To shed light on these questions, the C-More study was launched in the UK, focusing on the after-effects of the virus in patients who had been hospitalised.
Few studies on long COVID have looked at multiple organ harm in the same patient. And those that have, have tended to focus on patients who weren’t hospitalised with COVID. This makes our study unique. However, as with any pioneering study, there are some limitations.
The latest results, mentioned above, are based on preliminary data (interim analysis from half the study population). A complete analysis is still awaited.
Pre-COVID MRI scans from patients were not available, making definitive conclusions about the link between COVID and the organ changes difficult. The control participants were not an exact match to the patient population, but we adjusted our analyses to account for any differences, ensuring the findings were as accurate as possible.
The MRI scans didn’t always explain the symptoms experienced in individual organs. For instance, even if the MRI showed an organ to be normal, a patient could still exhibit related symptoms. The only strong tie identified was between lung abnormalities and chest tightness.
Still, this study was an important effort to better understand the long-term effects of COVID on multiple organ health. It reminds us to be vigilant of the potential for long-term consequences of the disease and the importance of vaccination – particularly in people at risk of severe infections.
Doctors and healthcare services around the world can now refine follow-up care, with a focus on lung, brain, kidney and blood vessel health among patients recovering from serious COVID infections, based on our study’s results.