|
Getting your Trinity Audio player ready...
|
Catherine Hudson drugged two patients on the stroke ward of Blackpool Victoria Hospital to give herself an easier life. She has been jailed for seven years and two months. Her colleague, Charlotte Wilmot, who conspired with her to drug a third patient, was given a three-year jail term.
The trial highlighted the easy access staff had to controlled drugs. The drug regimen on the stroke ward was described during the trial as “dysfunctional”. But why is this still happening? Wasn’t it all meant to have been sorted following the Shipman Inquiry?
Harold Shipman, a seemingly mild-mannered family doctor, was responsible for the deaths of over 200 of his patients over 23 years. The true horrors of his actions started to slowly unravel in September 1998 when he was arrested for the murder of one of his patients, 81-year-old Kathleen Grundy.
It was the vigilance of Grundy’s daughter, Angela Woodruff, that would set in motion a series of events that would ultimately bring an end to Shipman’s long-running killing spree that began in the 1970s. Until that point, he had been able to kill his patients undetected by being careful to cover up his tracks.
There was a collective denial by the British public that a family doctor could have harmed one of his patients, let alone many of them. Yet, at the conclusion of his murder trial in January 2000, Shipman was found guilty of the murder of 15 of his patients. The true number of his victims, however, is believed to be 215.
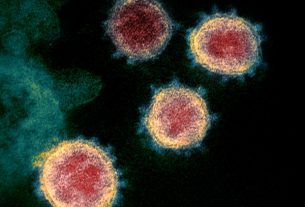
Most of the victims were elderly women and Shipman’s weapons of choice were the controlled drugs, diamorphine, morphine and pethidine – strong opioid painkillers.
Controlled drugs are those deemed by governments to pose a high risk to the public due to being addictive or harmful. Shipman administered these drugs to his patients in high doses. At the doses administered, the victims would have quickly lost consciousness and developed breathing difficulties before passing away.
Following Shipman’s conviction, governments around the world sought to ensure that their controlled drugs regulations were sufficient to prevent similar events in the future.
Shipman Inquiry
The Shipman Inquiry was set up by the British government in 2001 to understand how one person could have used controlled drugs so freely to harm their patients and to determine what procedures needed to be put in place to prevent another person doing the same again.
The inquiry recommended not only a cultural change within the medical and pharmaceutical professions, but also the need for new laws to protect the public.
In its fourth report, the Shipman Inquiry focused on the management and regulation of controlled drugs. It recommended better monitoring of them, with running balances being kept for the sale and supply of specific controlled drugs in controlled drug registers.
Wakefield Prison/Wikimedia Commons
In addition, a team of inspectors was to be appointed to check that controlled drug registers were being kept accurately, to track the prescribing of controlled drugs, and to monitor those who were prescribing them.
The inquiry recommended clamping down on self-prescribing and prescribing of controlled drugs for family members. It also limited the quantity that could be prescribed at any one time to a 28-day supply.
While the Shipman Inquiry only had oversight in the UK, its recommendations were relevant to an audience of global healthcare professionals and governments.
Still a problem
Despite all the changes, 25 years after Shipman’s arrest, controlled drugs are still a global problem.
While many of these medications have an important place in pain management, particularly for those with cancer, they are prone to abuse and misuse. In 2021 alone, the NHS spent over half a billion pounds on controlled drugs, and in the US, the opioid pandemic continues to rage, with people becoming addicted to opioid painkillers, like morphine and fentanyl, after obtaining them from registered prescribers.
The governance and oversight of controlled drug prescribing, in all healthcare settings, is still not as “robust as it should be”, according to the Care Quality Commission (CQC) in the UK.
It has suggested that digital tools, such as ePACT2, will allow authorised users to identify questionable prescribing of controlled drugs so that early interventions can be implemented to ensure safe care of patients.
In the US, prescription drug monitoring programmes are being used in a similar way to give real-time, controlled drug prescribing data to enhance care.
But just as these new tools come into play, more challenges are coming to light. The emergence of non-medical prescribers (paramedics, podiatrists, pharmacists, nurses, radiographers and physiotherapists) adds to the number of people who can prescribe controlled drugs, and, therefore potentially abuse and misuse them.
Winning the war on controlled drugs will continue to be a challenge. New drugs are brought to market every year, with the potential to cause harm and be categorised as controlled drugs. As such, the management of these drugs needs to remain fluid, with healthcare professionals and governments working together to protect the public from harm.