Understanding the most impactful 2023 healthcare statistics is critical if you’re in the healthcare industry or if you’re a customer of the U.S. healthcare industry — which is, basically, all of us. Young or old, employed or retired, what happens in healthcare affects us all.
Healthcare has been going through momentous changes. COVID changed everything, but the effects of an aging population, technology advances, labor shortages, and other trends that were happening even before COVID are also shaping healthcare in 2023.
2023 Healthcare Statistics — One Way or Another, This Will Affect Your Life!
1. About 30 percent of all rural hospitals are at risk of closing in the immediate or near future.
Rural hospitals have had a hard time for a while now, but this is just proof the end is not in sight. The closures will come as a result of ongoing financial losses hospitals have had to take on patient services, inadequate revenue, and insufficient financial reserves.
The consequences of this, of course, are considerable. Rural families will not have access to the care they need. They’ll have to travel further and further to get it, which means preventative care is less likely to happen.
2. A wave of hospital and healthcare facilities bankruptcies is expected in 2023.
Becker’s Hospital Review warns:
“Many hospitals and health systems are on course for their worst financial year in decades, and more hospital closures and bankruptcies could be on the cards next year, according to recent reports on the state of hospital finances in the United States.”
This can and will impact the level of care we’re all used to getting. It will also throw yet another wrench into the healthcare staffing picture and could also have significant impacts on how quickly nurses and other healthcare professionals can get the training needed to complete their certifications and degrees.
3. Soon, more Americans will get their healthcare from the government than from private firms.
158 million Americans (about half the country) are currently covered by Medicare, Medicaid, or they have subsidized enrollment from state and federal exchanges. This percentage is expected to increase enough that we will soon tip over into a situation where more people are insured by the government than by private firms.
4. Medical costs for the average US family have risen every year since 2000.
Has your company’s healthcare plan deductible increased significantly in the last few years? You’re not alone. Most companies have been shifting healthcare costs over to their employees, little by little, for some time now.
Just in 2022, U.S. employees paid 10.6% more in out-of-pocket healthcare expenses than they did in 2021.
This chart from StatNews illustrates the problem well:
Also, according to StatNews: “If nothing is done and health premiums continue to increase at the same rate, the average family premium will exceed $100,000 by 2046. If premiums and wages continue to increase at the same rates, the average family premium will overtake the average wage in 2055.”
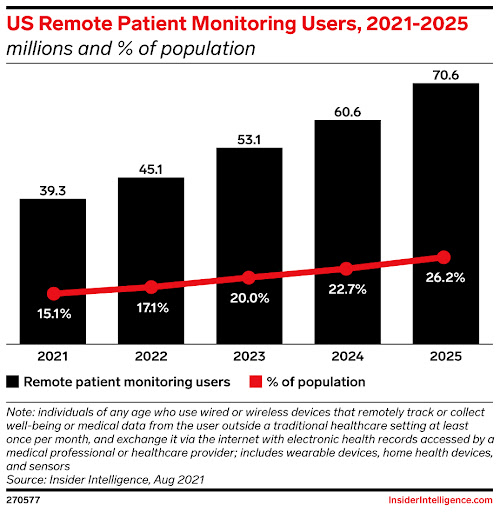
5. The use of remote patient monitoring (RPM) tools is becoming more widespread.
What if you could get medical tests done at home? What if all your neighbors could get tests done at home, too? It would mean a huge reduction in staffing, overhead costs, and patient transportation issues, and that’s just for starters.
This has begun to happen. And in the next few years, more and more people will be able to have their health conditions monitored without having to go to a clinic or a hospital. By 2024, over 75% of US medical practices are expected to be leveraging RPM technology.
These technologies could also be extremely effective in catching health issues early, which could, in turn, reduce the strain on the healthcare industry.
6. The U.S. will need more than 275,000 additional nurses within the next eight years.
You’ve probably heard about the nursing shortage. The problem is real — and it has direct consequences for how much care is available for ourselves or our families.
This is good news if you’re a travel nurse, as it means there will continue to be plenty of jobs and jobs that pay well. But it’s not such great news for hospitals: McKinsey’s analysis of the state of US healthcare repeatedly cites labor shortages as a factor impairing hospitals’ profitability.
7. 57% of nurses are comfortable using technology during their job searches, but they also want to work with recruiters.
This matters because of the labor shortage in nursing and in healthcare generally. There are a lot of positions to fill. We need to fill those positions if we’re going to provide care to everyone who needs it.
So while it’s great to set up online resources to help healthcare professionals find work, it’s also important to staff those nursing placement services with experienced recruiters who know how to match the right nurse with the right job. We need to give nurses and healthcare professionals the resources they need so they find work — and work that doesn’t burn them out.
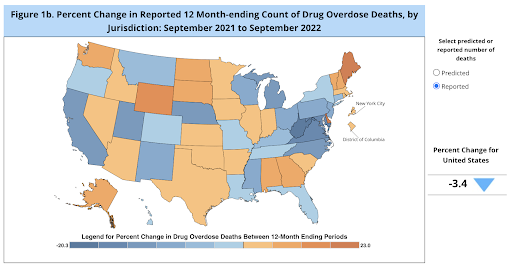
8. Drug overdose reported deaths have dropped slightly.
The scale of overdose deaths in the United States is still unprecedented — and insufficiently addressed. But there is a glimmer of hope in this healthcare statistic: Reported deaths are down, as reported by the CDC.
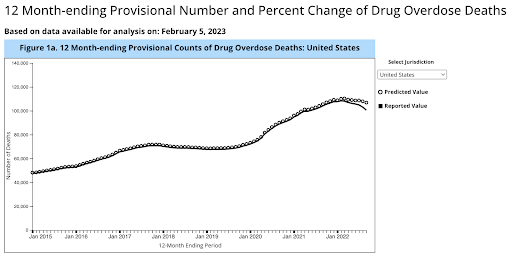
Depending on where you are in the U.S., you may or may not see this change. Several states — typically more rural states — are still in a full-scale crisis.
9. An aging population.
As of this year, one in every five Americans is over the age of 65. Caring for these older people will require more resources, more trained professionals, and more healthcare facilities than ever before. It will also lead to higher healthcare costs.
Once again, too: Just as this need for care is rising, the demographic shift towards an older populace means there will be fewer people, proportionally, to care for them. So once again, the nursing shortage and healthcare labor shortage will be an issue.
10. The mental health crisis.
You’ve probably heard a few mental healthcare statistics. They don’t paint a rosy picture:
• 1 in 5 Americans suffers from a mental illness.
• Almost 6 in 10 people with mental illness get no treatment or medication.
Teens, veterans, and women have been especially hard-hit by mental health issues in the last few years. But no demographic has escaped the problem. And once again, there are more patients than ever, but the healthcare infrastructure has been weakened at the same time as the need arose. More than 150 million Americans live in areas without enough mental health professionals.
Key takeaways from these ten healthcare statistics for 2023
There are some serious gaps in U.S. healthcare, and these aren’t going to go away any time soon. The drug crisis, mental health, COVID, and an aging population will continue to put enormous pressure on the U.S. healthcare system.
That system itself has gaps: There’s a shortage of nurses, we’re about to lose far too many rural hospitals, and all hospitals are struggling to stay profitable or at least break even. Pair hospitals’ profitability problems with the advancing costs of healthcare and healthcare premiums for U.S. families, and there’s obviously cause for concern.
Can technology fill those gaps? Not all of them, but it could help. Remote medicine leaped forward during the pandemic, and AI-driven medical advances will help it leap forward again. That might be enough to alleviate some of the issues we see in these healthcare statistics, but people will have to deliver the ultimate solution.
Featured Image Credit: Photo by Vidal Balielo Jr.; Pexels; Thank you!