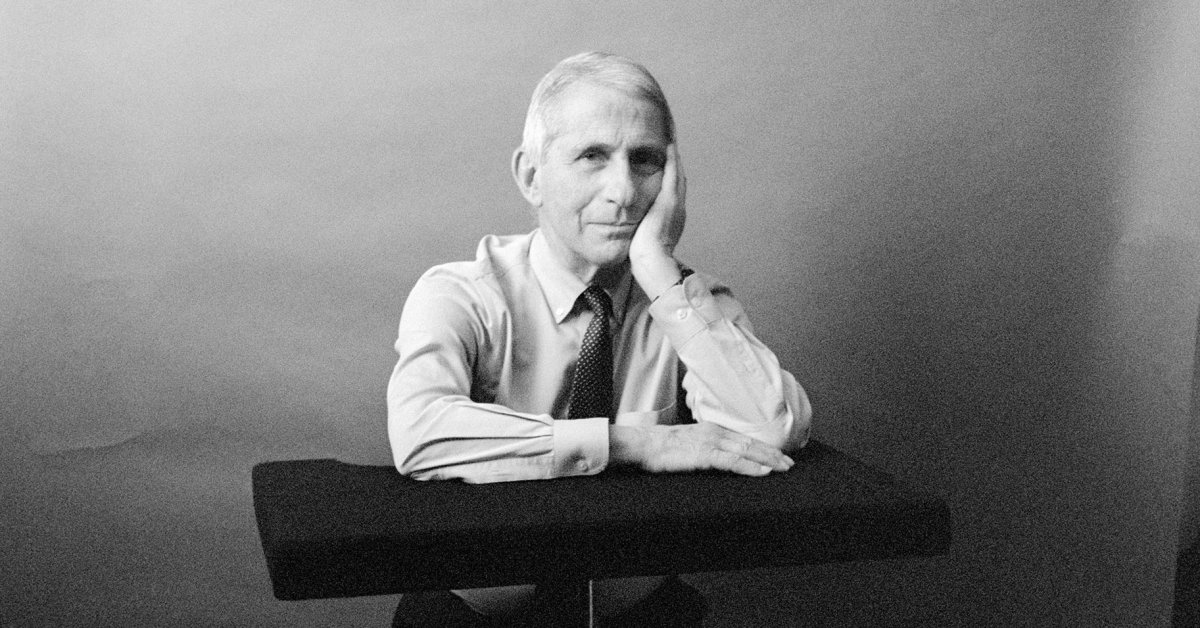
After Dr. Anthony Fauci steps down as head of the National Institute of Allergy and Infectious Diseases (NIAID) and chief medical advisor to President Biden on Dec. 31, he’ll leave behind a long and storied career. Ahead of his last day, he spoke to TIME from his office at the National Institutes of Health about what’s next for him—and his advice for whoever fills his shoes.
This interview has been edited and condensed for clarity.
TIME: You’re leaving your leadership positions in the federal government, but you aren’t retiring. What are you calling the next stage in your career?
Dr. Anthony Fauci: My wife jokingly calls it a rewiring. I would like to lecture and write, and advise to the extent that my advice is solicited. I have 54 years of experience as a scientist at the National Institutes of Health and 38 years running what everyone agrees is the largest and most important infectious-disease research institution in the world. And the privilege of advising seven Presidents of the United States over almost 40 years.
Could you reflect on what it was like to serve under each of those presidents?
When you look at the Reagan Administration, when I was first appointed we were trying very hard to get the administration to be a little bit more proactive in recognizing the seriousness of the HIV epidemic. That was just emerging at the time. That was a bit frustrating, because for all of the productive elements of that administration, the Reagan Administration still did not use the full bully pulpit capability of the presidency to call attention to the outbreak.
That changed somewhat with George H. W. Bush, whom I got to know personally very well. Even though there’s been criticisms—”did he do enough?”—he really changed things a lot. That’s when the budget of the NIH really went up with the help of Congressional support.
Clinton opened up much more accessibility of different constituency groups—the LGBT community and others—to have a say in what went on.
George W. Bush, when it comes to HIV/AIDS, in my mind, has had the most impact of anybody. He gave me the privilege and the honor of being one of the architects of the President’s Emergency Program for AIDS Relief (PEPFAR) program, which, as we know, saved more than 20 million lives.
Then we went to Obama, who was someone in my mind who handled crises very well. We had pandemic flu, we had Ebola, we had Zika.
The Trump Administration—it’s very clear that there were difficulties there, because I had to be put in a position of having to contradict the president for things that he had said in the impression that he was giving: that the virus was going to disappear like magic. I just felt I owed my responsibility to the American public to stand up for the data and evidence and facts and science. That put me in a very uncomfortable position of having a lot of opposition to me, which has now continued on to this day.
Then, things got back to science in the current administration with Biden, who made it very clear that he wanted science to be the thing that guided us. He knew that we’re not going get everything right, but we’re going to try our best.
You began your career as a target of criticism by the HIV activists in the 1980s and are ending it with a bullseye on your back again during COVID-19. How did your earlier experience help you recently?
People talk about the bookends of my career, and they show pictures of the AIDS activists storming the NIH campus, saying, “You’re killing us, you’re not listening to us.” And then they show pictures of people in today’s environment saying, “Hang him, cut his head off, execute him,” things like that. The differences there are so profound. Back then, the activists were trying to call attention to the rigidity of the federal government in its scientific clinical trial approach and its regulatory approach. They were iconoclastic, they were disruptive, they were theatrical. One of the best things I did in my entire life was to look at what they were doing and listen to what they were saying. And they were making sense; I would’ve done the same thing if I were in their shoes. It went from confrontation to collaboration, to cooperation, to actual friendship, because they were absolutely correct, and the system needed to be changed. So the end game for them was good. I would never, ever feel threatened, no matter how much they were demonstrating against us.
What we’re dealing with today is a reflection of the divisiveness in society where people talk about things that are patently untrue conspiracy theories, a normalization of untruth, which is very dangerous. Because when society shrugs their shoulders and accepts the fact that people can just say things that are patently false and get away with it, and then social media amplifies it, sooner or later, people can’t figure out what’s right and what’s wrong. Not only is that dangerous to public health, that’s dangerous for our own democracy.
During that time, science has come in and out of favor with the public. How important is it for the public to understand and appreciate science?
We’re dealing, unfortunately, with somewhat of an antiscience theme in this country, which is reflected by antivax movements and things like that. Political ideation has been very disruptive to the kind of cooperation and collaboration that you need for public health. If there’s one area where you would really like to have everyone pulling together, it would be as we confront a historic pandemic such as COVID-19. But that’s not what we’re seeing. We’re seeing fundamental public-health principles being interpreted one way or the other, depending upon what your political ideology is.
You and your family have required personal security after threats from critics of the COVID-19 response. Did you ever question whether continuing was the right thing to do?
That never deterred me for a moment. I would never, ever let that kind of a threat from people who are cowards deter me from what I felt my mission is. What bothers me more than anything is the cowardice of people who harass and threaten my wife and my children.
What advice would you have for your successor?
Stick with the science. No. 1, always go with the data, with the evidence. And although you may be involved in policy, stay out of politics. Do not at all show any ideology one way or the other. Just be a pure scientist. That’s what you need in the job.
What do you predict COVID-19 will look like in coming years?
We don’t know for sure, but I can give you what I think are some reasonable projections. Unless we get a surprise with a way-out-there, totally different variant, we will have greater control as more people get vaccinated or wind up getting infected. If you get vaccinated and then get infected, the chances of you getting a serious outcome are very, very low. We will get little blips and surges, but we’re hoping that it never gets to that level where it really disrupts the social order. We may need an updated SARS-CoV-2 booster every year, similar to the flu vaccine.
Your career has been a series of skirmishes with a variety of pathogens. Which foe has surprised you the most?
HIV and COVID-19 are up there. HIV came on insidiously, and over 40 years [later], we’re still dealing with it. It was mysterious in the beginning. I was taking care of patients for three years knowing they’re dying in front of me, but not knowing what the agent is that’s killing them. That is a unique and terrible experience as a physician that I will never, ever shake. Thank goodness we developed lifesaving drugs so that now people living with HIV can live essentially a normal lifespan.
[With] COVID-19, I never would’ve thought it was going to be prolonged like this and have so many variants. I was hoping in the beginning when it was so bad, it would be a one-off—we’d have a big blast, and then it would come down. But that’s not what happened. It’s been a terrible ride ever since.
As you step down from leading NIAID, is there any unfinished business you leave behind?
Oh, absolutely. There is always unfinished business. We need to get a vaccine for HIV. It’s going to be a very formidable scientific challenge, but we need to continue to push the envelope and try to get there. Perhaps even a cure for HIV, which I think is going be even more aspirational, but it’s not out of the question. Also, there are big killers throughout the world for which we don’t have highly effective vaccines yet—specifically malaria and tuberculosis. Not to mention the perpetual threat of a new emerging infection.
Looking back on your career, what achievement are you are most proud of?
Well, I wear three hats and I have achievements in all three that I feel good about. Others will judge how important they are. I’ve devoted my scientific career early on to developing cures for inflammatory vasculitis diseases, although they’re rare. The therapies that I developed have transformed those diseases. I also spent 41 years studying the pathogenic mechanisms of HIV, and together with a lot of other really good investigators throughout the country, we’ve made some good contributions.
Then, as director of NIAID, the thing I’m proud of the most is developing and creating the AIDS program, which, together with the pharmaceutical companies, was responsible for developing the combinations of drugs that now clearly have saved millions of lives. I don’t take credit for that alone, but as the director of the institute, I feel proud to have played a major role in that.
Policy-wise, maybe the most impactful of anything I’ve done was to have the privilege that was given to me by President George W. Bush to be the architect of the PEPFAR program.
And things that you aren’t so proud of?
I’m far from perfect. But there isn’t anything I’m ashamed of at all. There are so many things I could have done better. One of those things was early on in HIV, the people in classic infectious diseases were reluctant to use prophylaxis [to prevent opportunistic infections], because we felt it would have some harm to it, and it would lead to resistance of the pathogen. Now, that’s an integral part of treating somebody with advanced HIV. I felt we should have probably started that a little bit earlier than we did. But again, we acted on the data that we had at the time. So it’s nothing that I’m ashamed of, but I think we could have done it better.
What are your plans for the first day you are no longer head of NIAID?
Probably sleep an extra hour and not get up at five o’clock in the morning the way I have for the last 40 years. That’s the first thing I will do.
More Must-Reads From TIME