Diabetes is a global health problem. Those who suffer from this disease produce little or no insulin, or have an ineffective response to insulin that causes their high blood sugar levels to be abnormally high.
Among the different types of diabetes, type 1 is most common in childhood and adolescence – in 2019, about 1.5 million people under 20 years of age were affected worldwide, and of the 16,300 deaths attributed to diabetes in people under 25 years of age, 73.7 % were caused by type 1 diabetes.
Despite recent progress, managing this disease is still a challenge for health systems around the world.
A massive childhood health issue
Type 1 diabetes is a chronic autoimmune disease in which the immune system attacks and destroys the cells in the pancreas that produce insulin. To make up for the deficiency, patients have to be supplied with insulin through injections or delivery devices such as insulin pumps.
In addition, people with diabetes need to monitor their blood sugar, as well as manage nutritional intake (especially carbohydrates), physical activity and other factors that can alter blood glucose levels.
Poor management of the disease raises blood sugar. Over time, this can affect or damage the body’s main organs, including the heart, blood vessels, nerves, eyes and kidneys.
It is therefore crucial to understand the evolution of the number of young people suffering from this disease in order to identify its causes, and to provide health officials with data that will help identify new cases as early as possible.
Case numbers have almost doubled
To provide this much needed information, we examined the incidence – meaning the proportion of new cases of a disease over a period of time in relation to the population likely to suffer from it – of type 1 diabetes in 32 European countries from 1994 to 2021. To do this, we analysed a total of 75 studies, covering 219,331 individuals aged 0 to 14.
We found that the incidence of type 1 diabetes has increased considerably: from 11 cases per 100,000 person-years between 1994 and 2003, to approximately 21 cases per 100,000 person-years between 2013 and 2021.
Differences among countries
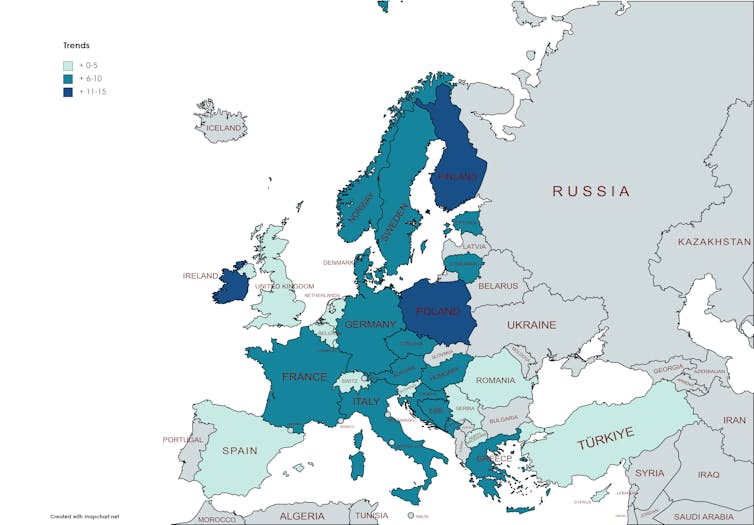
In addition, we identified significant differences among European regions. While there is a clear upward trend in most European countries – especially those in Northern Europe, such as Finland, Sweden and Norway – numbers seem to have stabilised in some, including the United Kingdom and Spain.
Between 2013 and 2021, the latest period studied, the lowest incidence rates were in Romania and Turkey (11 and 12 cases per 100 000 person-years, respectively), and the highest in Finland and Ireland (56 and 33 cases).
In Spain, the numbers have risen less sharply. In the period from 1994 to 2003, there were 16 cases per 100 000 person-years, rising only slightly to 17.5 between 2013 and 2022.
Across Europe, boys showed slightly higher figures than girls. We also observed that incidence rates increased with age, especially in the 10-14 age group.
What’s behind these rising numbers?
The origin of type 1 diabetes is still unknown, although some lines of research indicate that there is a genetic predisposition. Other triggers have also been suggested, including autoimmune processes, viruses, and lifestyle or environmental factors such as diet.
We have also observed that a higher per capita income or living in a more northern country, such as Finland, Sweden or Norway, could affect the incidence of type 1 diabetes.
There are several possible explanations for this, including the fact that northern countries receive less ultraviolet radiation (i.e. sunlight) – several studies have found that exposure to ultraviolet radiation may protect against diabetes, as it appears to slow down the body’s immune reactions.
The pandemic effect
Another noteworthy point is the worldwide increase in new cases of type 1 diabetes in children since the covid-19 pandemic.
This could be the result of infection impacting the immunity of people vulnerable to the disease, or because of health systems’ reduced capacity to detect the problem early and keep it under control.
Currently, further work is needed on health policies that promote healthy lifestyles, and that control the environmental risk factors which sit at the root of the immune problems that are related to this major public health challenge.



