Today’s NHS faces severe time constraints, with the risk of short consultations and concerns about the risk of misdiagnosis or delayed care. These challenges are compounded by limited resources and overstretched staff that results in protracted patient wait times and generic treatment strategies.
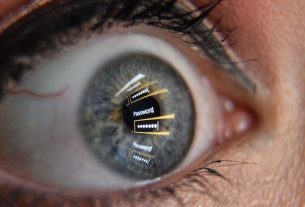
Staff can operate with a surface level view of patient data, relying on basic medical histories and recent test results. This lack of comprehensive data interferes with their ability to fully understand patient needs and compromises the accuracy and individualisation of diagnoses and treatments. Such a healthcare approach, characterised by these limitations and engagements, could aptly be termed “shallow medicine”.
The American cardiologist and scientist Eric Topol introduced the concept of “deep medicine” in his 2019 book Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. He critiques the US’s shallow medicine model, offering insights from his clinical and personal experiences.
Deep medicine holds the potential to revolutionise medical diagnostics, the effectiveness of treatments, and operational considerations. Topol presents artificial intelligence (AI) as the transformative solution to these systemic shallow issues. He outlines what he calls the deep medicine framework as a comprehensive strategy for the incorporation of AI into different aspects of healthcare.
The framework of deep medicine is built upon three core pillars: deep phenotyping, deep learning and deep empathy. These pillars are all interconnected and adopting this framework could enhance patient care, support healthcare staff and strengthen the entire NHS system.
Deep phenotyping
Deep phenotyping refers to a comprehensive picture of an individual’s health data, across a full lifetime. A deep phenotype goes far beyond the limited data collected during a standard medical appointment or health episode. It includes things such as a person’s genetic code, the entirety of an individual’s DNA, and information about the body’s microbes or microbiome.
It encompasses what’s known as the “exposome”, the things in the environment that a person is exposed to during life, such as air pollution. It includes markers that reveal details of the metabolic processes going on in a person’s body and the proteins their body is expressing, as well as other biological measures and metrics. It comprises a person’s electronic health records, including their medical history, diagnoses, treatments and lab results.
Deep learning
The philosophy underpinning deep phenotyping is to combine this diverse data to enable more accurate and speedy diagnoses, precise and effective treatments, and to advance predictive and preventative medicine strategies. However, the sheer volume and complexity of the collected data pose significant challenges for analysing it all. This is where deep learning – an area of AI that seeks to simulate the decision-making power of the human brain – is so valuable. Deep learning uses an algorithm called a neural network that uses little, mathematical computers, called “neurons”, that are connected to one another to share and learn information.
Elif Bayraktar / Shutterstock
Advances in neural network algorithms, technology, and availability of digital data have enabled neural networks to demonstrate impressive performance. For instance, they have enabled the rapid and accurate analysis of medical images, such as X-rays and MRIs. They can generate reports and predict disease progression and outcomes for the patient.
AI is proving valuable in drug discovery and the identification of chemical markers from the body, such as those that can signal the presence of cancer. They can control instruments used in robotic surgery. In addition, AI technology like that behind ChatGPT can process medical literature and patient records to help make complex diagnoses. They can automate writing tasks, such as note taking and data entry.
Deep empathy
Integrating AI systems could help streamline operational tasks in health services like the NHS. These include bed management and hospital workflows. However, the development of AI technologies should not be haphazard – rather it needs to be targeted at real clinical needs and designed to foster better relations between patients and staff. This is the pillar of deep medicine known as deep empathy.
Healthcare has increasingly become a discipline where the human touch, once its cornerstone, is overshadowed by a relentless pursuit of efficiency. Healthcare staff face an increased burden of administrative tasks. This can reduce the time they devote to each patient, eroding the essence and potential benefits of compassionate care.
Staff need the sensitivity and time to respond to the emotional and psychological needs of patients and their families. This nurtures a supportive and compassionate care environment, and strengthens the human connection at the heart of healthcare.
AI solutions can be designed to reduce the administrative burdens for staff, opening up more opportunities for meaningful patient interaction. By removing these barriers, we allow for a greater focus on direct patient care, helping improve the quality of the service provided and, hopefully, patient satisfaction.
There is also a transformative opportunity to rethink efficiency, putting relationships between patients and staff at the core. It envisions a future where healthcare staff excel in both technical skill and emotional intelligence, enabling them to meet the psychological needs of patients with genuine understanding and compassion.