Spain performs more than half of all egg donation treatments across Europe. The country is the largest provider of donor eggs across the continent. And every year, thousands of international fertility patients travel to Spain to access treatments.
Spain is a popular choice for private fertility treatments because any woman or man regardless of their civil status, sexual orientation or age can access them. Indeed, many come to Spain because of restrictions and bans in their home countries, particularly related to egg donation. Spain also tends to have very short waiting lists.
At the same time, egg banks in Spain have proliferated in recent years, shipping donor eggs around the world, as part of this multi-million-pound industry.
Close to 15,000 women undergo egg extraction cycles every year in Spain. Many are financially motivated – donors in Spain receive one of the highest rates of financial compensation across Europe (around €1,100 (£945) for a successful cycle).
This article is part of Women’s Health Matters, a series about the health and wellbeing of women and girls around the world. From menopause to miscarriage, pleasure to pain the articles in this series will delve into the full spectrum of women’s health issues to provide valuable information, insights and resources for women of all ages.
You may be interested in:
The orgasm gap and why women climax less than men
Five old contraception methods that show why the pill was a medical breakthrough
While research has previously shown that some women claim to give their eggs for altruistic reasons (often alongside financial motivation), very little is known about women’s experiences of egg donation. They are for the most part invisible. This is why I wanted to find out more about what it’s like being an egg donor in Spain.
As part of my research, I interviewed egg donors and doctors and also observed women in fertility clinics to get a better sense of what the process was actually like.
The reality of egg donation
Fertility clinics’ websites usually describe egg donation as a fast and easy procedure. But women wanting to become egg donors have to do a fair bit of preparation before the donation can actually take place.
First, a screening happens which includes health-related and psychological questionnaires as well as gynaecological and genetic tests. Potential donors will then be given hormone injections for about ten days.
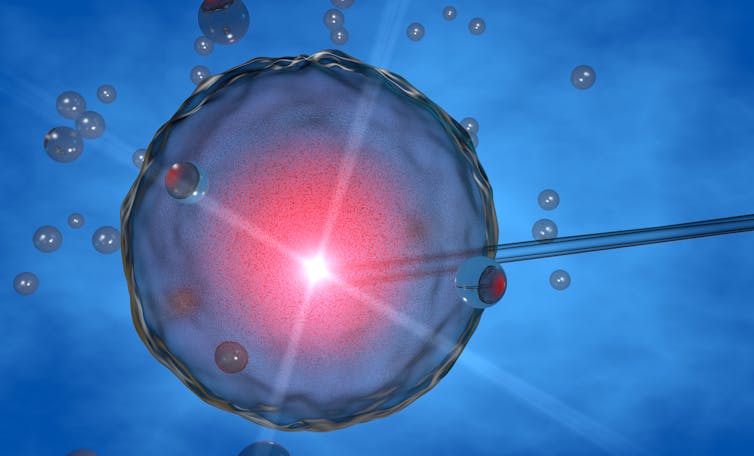
After that, egg retrieval occurs which involves surgery under general anaesthetic to remove the eggs through a vaginal ultrasound scanner which is connected to a needle. It’s a time-consuming, inconvenient and at times painful process.
It also carries medical risks such as ovarian hyperstimulation syndrome, which is when the ovaries become enlarged and can lead to several serious problems such as blood clots or bleeding.
Donors can also experience medication intolerance or side-effects alongside a risk of infection during surgery. But the longer-term risks of being an egg donor remain largely unknown, because of the limited amount of studies carried out in this area.

HealthyCapture Studio/Shutterstock
I also discovered that the reality of egg donation can mean busy schedules balanced between work, studies and personal life. To avoid losing any income, most of the women I spoke to didn’t usually stop any of their usual activities during the cycle. Instead, they tried to make it all fit into their busy lives – which sometimes created risks in terms of their health.
This was particularly obvious when it came to the egg extraction. The scheduling of the surgery relies on the pace of the hormonal drugs in the body, so it cannot be decided according to the donors’ convenience. When the eggs are ready to be collected they are ready to be collected – and this can differ from patient to patient. When donors are ready, they have to administer the final injection, which is the one that makes them ovulate before they are scheduled for the surgery the next morning.
The result is that although clinics advise resting for 24-48 hours after the extraction, many egg donors work the next day, or even the same day, on their afternoon shifts.
Payments and compensation
Compensation for a cycle is usually paid in cash at the end of the process. And is only secured after the extraction surgery if there are extractable eggs – donors are paid the same amount regardless of the number of eggs.
If the process has to be stopped before the extraction for reasons that aren’t the donor’s fault, such as the medication not producing the expected effects on egg production, most clinics do not offer compensation.
If donors undergo the extraction surgery but there are no extractable eggs, the matter is usually discussed among doctors, with significant differences across clinics. If there is an indication that the donor may not have administrated the last injection of hormones or that she did so at the wrong time, the clinic will usually not pay her at all.
If the clinic believes she followed the rules but that she ovulated earlier than expected, different clinics have different rules: some might give her the full amount, others only a partial payment and some nothing at all.
Donors may also be required to reimburse all expenses for the treatments if they decide to abandon the process halfway through for non-medical reasons – something most can’t afford to do.
In the event of side effects or complications following the extraction, donors are usually referred to the emergency room of public hospitals, as the donation contract does not include private health insurance.
Naeblys/Shutterstock
The few studies on egg donors’ experiences in Spain that do exist show problems and gaps in terms of the information donors are provided with and the conditions in which egg donation is undertaken.
Most of the women I spoke to didn’t know how many eggs were extracted, the number of women that might be treated with them, or whether they will be used in the clinic, frozen to be banked or shipped abroad.
It is clear then that as the demand for egg donation increases, urgent action is needed to ensure that women in the global egg donation industry are properly informed, cared for and insured in case of complications and side-effects.



