In 1990, Fried Vancraen visited a German trade show and was captivated by a 3D printer displayed there – so much so that he bought one for his new company, Materialise. Two years later, with the help of EU funding, he took his small Belgian start-up on a journey that would change the world of medicine – and 3D printing – forever.
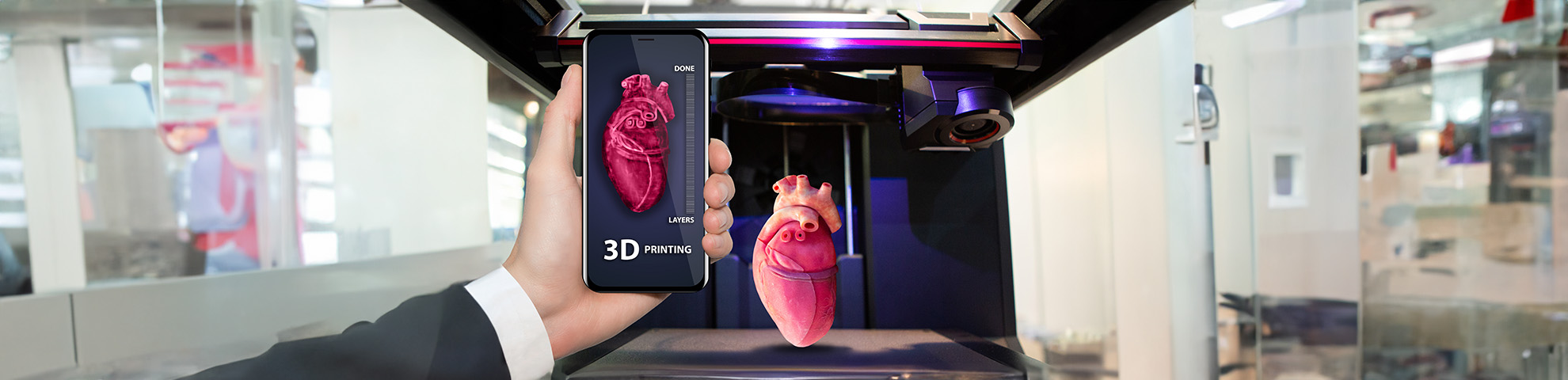
Vancraen and Materialise pioneered the use of 3D printing for medical purposes, with partners from Germany and the UK. For the first time they started producing accurate, tangible models of human bones and organs, based on medical images. This provided immense help for surgeons planning complex procedures.
“Already then, we were convinced 3D printers would change the medical world,” he said.
After Materialise went from a university spin-off to a multinational enterprise, Vancraen retired from the executive position in 2024 to become company chairman. But he still vividly remembers the excitement of embarking on a new chapter to test their ideas more than 30 years ago.
What helped them start along this path was an EU grant for their research project called PHIDIAS. It ran for three years, until the end of 1995, and focused on producing accurate medical models based on improved medical images, mostly computed tomography (CT).
“Of course I remember it,” Vancraen exclaimed when asked about it. “I was the project manager, I wrote the [funding] proposal and I brought together the partners.”
“
Today, we 3D-print implants customised for the patient.
They included Imperial Chemical Industries from the UK, whose pharmaceutical arm went on to become a separate company, Zeneca, in 1993, as well as Siemens, the industrial giant from Germany that manufactured medical imaging devices, and KU Leuven University in Belgium.
Having started as an offshoot of KU Leuven, Materialise now employs around 2 000 people and is listed on the Nasdaq stock exchange in New York.
Meanwhile, 3D printing has become a cornerstone of surgical healthcare. 3D printers are regularly used to make implants, prosthetics and models of a patient’s body on which surgeons can train.
When Materialise started, however, the technology was in its early days. There were doubts about how useful it could be and whether doctors could use it to treat real patients.
Work started in earnest on 1 January 1993, less than three years after the company was founded.
“Those were our start-up days,” said Vancrean. “We had a team of around 20 people at the time.”
From salami sausage to spiral scan
For Vancraen’s team, the first priority was to improve medical imaging.
“Taking a CT scan at the time was like cutting a salami,” Vancraen remembered. “To make the scan, the scanner would make an image of one layer of the patient’s body and then be moved forward a few centimetres to make another scan – just like you would slice a sausage.”
“Every time the patient moved, even in the slightest, you would get issues in the image,” Vancraen said, referring to the so-called artefacts, unintended patterns or distortions in the imaging.
3D printing requires accurate images of the patient’s body. If, for example, you want to 3D-print an implant that will seamlessly fit, you need the exact image of the patient’s body. Artefacts in the scan will mean medical issues and discomfort for patients later on.
This is why the team around Materialise replaced the “salami method” with a spiral CT scan. “We managed to scan the patient in one movement,” said Vancraen. “The CT would move in a spiral around them.”
Another hurdle was cleared when Zeneca, which later merged with Sweden’s drugs firm Astra to form AstraZeneca, developed a human-compatible polymer that was 3D-printable. This replaced older polymers that were often toxic for humans and could not be used for implants.
Walking before running
Seeking to scale up their pioneering technique, Materialise took their technology to the university hospital of Leuven, their hometown. There they tested whether surgeons could actually benefit from 3D printing, working closely with 30 surgeons from Belgium, France, Germany and the US.
“We did the first real clinical study on 3D printing in healthcare,” said Vancraen. In particular, they helped surgeons prepare for complex surgery.
His team used laser stereolithography, a technique that prints complex, accurate models layer by layer. It works by focusing an ultraviolet laser on resin made of large molecules sensitive to UV light, with the help of computer-aided design software.
Using their new scanners that were able to produce better medical imaging, they made 3D-printed models of organs and body parts the surgeons would operate on. This way, surgeons could prepare for what they would encounter inside the patient’s body and adjust their approach.
“In several cases, we managed to reduce the number of surgeries a patient had to go through,” said Vancraen.
“One person had three surgeries planned. Because of our technology, the surgeon could plan them better and actually complete the procedure in one surgery. That reduced the impact on their body tremendously.”
By combining improved scanning and printing, PHIDIAS was the team who laid the foundation for future advances in medical 3D printing.
“We needed to learn how to walk before we could learn how to run,” said Vancraen. “PHIDIAS was the moment we learned how to walk.”
Stepping stone
One of the researchers doing the running at Materialise today is Roel Wirix-Speetjens, a medical research manager. He develops new solutions that build on the work done by PHIDIAS researchers.
“PHIDIAS created our medical division,” he said. “Since then, we have, for example, delivered more than 400 000 customised knee instruments. That’s something I’m very proud of,” he said, referring to aid pieces that help surgeons work more accurately.
In one project, Materialise managed to make a detailed 3D model of a patient’s lungs, including the airway tree and lung lobes, or sections of each lung. This model helps surgeons who need to remove lung cancer by allowing them to pinpoint the exact location of the tumour.
“
In several cases, we managed to reduce the number of surgeries a patient had to go through.
“In this way, they remove less of the healthy lung tissue,” said Wirix-Speetjens. “That makes the patient’s recovery much less intense.”
But they are also developing new 3D printing technologies. Among other things, Materialise has designed ways to improve facial surgery.
In the past, if a patient suffered, for example, an injury that deformed their face, surgeons had to use standard implants to replace the damaged bone and tissue. They had to manually bend the implants during surgery to make them interlock with the remaining facial structure.
“Today, we 3D-print implants customised for the patient,” said Wirix-Speetjens. “We scan their faces and our 3D printers make intricate implants that allow surgeons to reconstruct the facial structure.”
Treatment can now be customised to the needs of an individual. PHIDIAS was a key step in making that possible, with exciting opportunities still ahead.
“We have only been doing this for 34 years,” said Vancraen. “I don’t know where we will end up.”
Research in this article was funded by the EU’s Framework Programme. The views of the interviewees don’t necessarily reflect those of the European Commission. If you liked this article, please consider sharing it on social media.